研究主題- 脈衝射頻在生醫領域之應用
撰寫:學生陳冠彬
脈衝射頻(Pulsed Radio-frequency, PRF)在醫學領域中被廣泛用於不同的應用,包括疼痛管理和神經系統疾病治療。PRF是一種電刺激技術,可以有效地控制或減輕疼痛感,但它的應用不僅限於此。下面將介紹林啟萬教授的幾項研究,它們展示了PRF在不同領域的應用和潛力。
第一項研究2010年發表在ISSCC [1],其中使用了無電池的單晶片系統互補型場效電晶體( CMOS SoC ) 來實施低電壓PRF刺激。這項研究的目標是觀察白老鼠接受PRF刺激後的行為,以證明其有效性。通過在腰神經節(Dorsal root ganglion , DRG)上施加局部刺激,成功地實現了疼痛控制,而不會引起熱損傷。這項研究的結果為使用PRF技術處理疼痛問題提供了新的思路。
另一項研究2017年發表在Neurourology and Urodynamics [2],關注了PRF對膀胱功能的影響。膀胱過度活動是一種常見的疾病,通常難以治療。而在此項研究中,藉由觀察在白老鼠的惡骨神經和骨盆神經上施加PRF電刺激發現可以顯著改善膀胱功能,而且不會對神經造成明顯的損傷!
最後一項研究探討了在創傷性腦損傷( Traumatic brain injury, TBI )患者中使用深腦刺激( Deep brain stimulation, DBS )治療膀胱功能障礙的可能性。此研究分別發表在2018年的Journal of Medical and Biological Engineering以及2019年的Neuromodulation: Technology at the Neural Interface [3, 4]。TBI通常會導致永久性腦組織損傷,進而引發膀胱問題。標準治療方法難以緩解癥狀,因此研究人員嘗試了DBS技術。林教授的團隊開發了一個閉環控制的DBS系統,並在TBI動物模型中測試了其效果。結果顯示,DBS可以顯著改善排尿功能,但會伴隨運動功能的惡化。這項研究的成果為未來開發植入式膀胱控制器提供了基礎。
總的來說,PRF技術在不同領域中顯示出廣泛的潛在應用價值,包括疼痛管理、膀胱功能恢復以及神經系統疾病治療。這些研究為利用PRF技術來改善患者生活品質提供了新的希望,並為未來的臨床應用提供了有益的資訊。
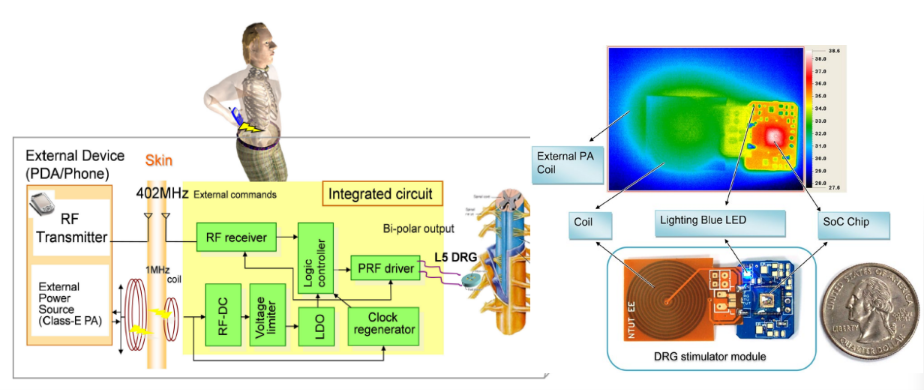
圖一、利用低電壓PRF來減緩疼痛
Pain control by low-voltage PRF stimulation
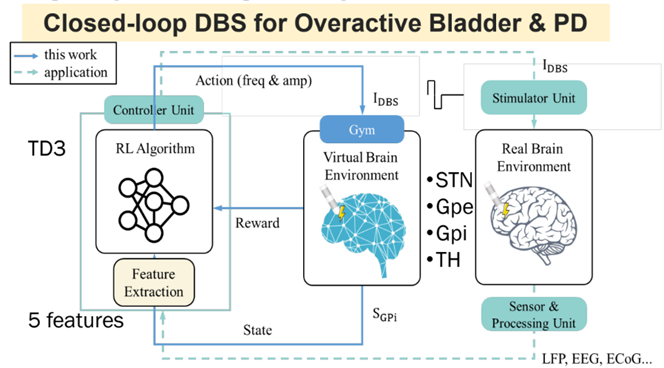
圖二、閉環控制的DBS以治療TBI
Closed-loop DBS for overactive bladder & PD
Pulsed Radio-frequency (PRF) is widely used in the medical field for various applications, including pain management and the treatment of neurological disorders. PRF is an electrical stimulation technique that can effectively control or alleviate pain, but its applications go beyond that. Below, we will introduce several studies conducted by Professor Chii-Wann Lin, which demonstrate the applications and potential of PRF in different areas.
The first study, published in ISSCC in 2010, utilized a batteryless CMOS SoC to implement low-voltage PRF stimulation. The objective of this study was to observe the behavior of rats after receiving PRF stimulation to demonstrate its effectiveness. By applying local stimulation to the Dorsal Root Ganglion (DRG), pain control was successfully achieved without causing thermal damage. The results of this study provide new insights into using PRF technology to address pain-related issues.
Another study, published in Neurourology and Urodynamics in 2017, focused on the impact of PRF on bladder function. Overactive bladder is a common condition that is often challenging to treat. However, in this study, it was observed that PRF electrical stimulation applied to the pudendal and pelvic nerves in rats significantly improved bladder function without causing significant nerve damage!
The last study explored the possibility of using Deep Brain Stimulation (DBS) to treat bladder dysfunction in patients with Traumatic Brain Injury (TBI). These studies were published in the Journal of Medical and Biological Engineering in 2018 and Neuromodulation: Technology at the Neural Interface in 2019, respectively. TBI typically results in permanent brain tissue damage, leading to bladder problems. Standard treatment methods often do not relieve symptoms, prompting researchers to investigate DBS technology. Professor Lin’s team developed a closed-loop control DBS system and tested its effectiveness in a TBI animal model. The results showed that DBS significantly improved urinary function but was accompanied by a deterioration in motor function. The findings from this study provide a foundation for the future development of implantable bladder controllers.
In summary, PRF technology has demonstrated extensive potential applications in various fields, including pain management, bladder function restoration, and the treatment of neurological disorders. These studies offer new hope for improving the quality of life for patients using PRF technology and provide valuable insights for future clinical applications.
Ref:
[1] C. W. Lin et al., “Pain control on demand based on pulsed radio-frequency stimulation of the dorsal root ganglion using a batteryless implantable CMOS SoC,” in 2010 IEEE International Solid-State Circuits Conference – (ISSCC), 7-11 Feb. 2010 2010, pp. 234-235, doi: 10.1109/ISSCC.2010.5433936. [2] E. Jen et al., “Effects of pulsed-radiofrequency neuromodulation on the rat with overactive bladder,” Neurourology and Urodynamics, vol. 36, no. 7, pp. 1734-1741, 2017, doi: https://doi.org/10.1002/nau.23183. [3] E. Jen et al., “Prototype Deep Brain Stimulation System with Closed-Loop Control Feedback for Modulating Bladder Functions in Traumatic Brain Injured Animals,” Journal of Medical and Biological Engineering, vol. 38, no. 3, pp. 337-349, 2018/06/01 2018, doi: 10.1007/s40846-017-0326-1. [4] C.-H. Chang, K.-H. Lu, W.-T. Lin, S.-C. Chen, W.-P. Shih, and C.-W. Lin, “Reversible Spasticity Suppression and Locomotion Change After Pulsed Radiofrequency on the Dorsal Root Ganglia of Rats With Spinal Cord Injury,” Neuromodulation: Technology at the Neural Interface, vol. 22, no. 1, pp. 53-60, 2019/01/01/ 2019, doi: https://doi.org/10.1111/ner.12853.